
The Asymmetrical tonic neck reflex (ATNR) is a primitive reflex that is found in new born babies and normally remains until around 6 months. It emerges in utero at around 18 weeks after conception and is usually identified and seen within the first 3 months after birth. The reflex is initiated when the head is turned to the left or the right whilst the baby lies on its back. The turning of the head causes the arm and the leg on one side to extend, whilst the limbs on the opposite side flex. If the head turns to the right, the right arm and leg will automatically extend whilst the left arm and leg both flex. It is often called the "fencing" reflex due to this pattern.
The purpose of the ATNR is to provide stimulation for developing muscle tone and the vestibular system whilst in the womb before birth. It also assist with the birthing process by inhibiting limb movement and slowing it down so that the baby uses a "corkscrew" movement through the birth passage. ATNR helps with eye-hand co-ordination and serves as a precursor to this skill. A retained ATNR can have a significant impact on a child's development and it is often thought to have a major effect on the child's physical, cognitive, social and emotional progress, thus affecting their ability to function well in school. The retained reflex will continue to influence limb movement every time the head is turned and will have physical influences that impact on all other areas.
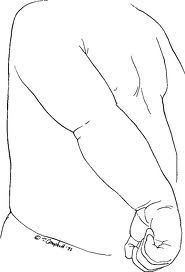
The ATNR will interfere with a baby's ability to centralise and reach things within the mid line position of their body. Once this reflex is integrated (around 6 months) the baby begins to reach and have functional ability within the mid line of their body. A strongly retained ATNR will affect this ability so that the baby finds it difficult for hands, feet and eyes to cross the mid line. Visual tracking and eye pursuit of an object becomes difficult and this later results in difficulty with reading as the child can not easily make the rapid forwards and backwards eye movements (saccades) that are essential for reading. Writing will also be difficult due to this as well as due to the reflex causing the hand to involuntarily extend as the head is turned towards the hand. The child will find it difficult to maintain a pen grip and may compensate with a lot of pressure in a tight grip, causing cramps and making their writing messy and illegible. The child may also find it difficult to copy written work as their eyes will follow their hand and not the text.

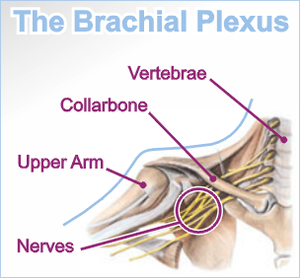
The retained ATNR prevents a baby from developing certain physical cross pattern movements such as rolling over, crawling and later marching using alternative leg and arm. As they grow older the child may have atypical movement patterns and may draw circles backwards, clap downwards, use one hand more than the other whilst clapping, or may be very single handed in most activities. A strongly retained reflex in the legs can also affect balance as the child looks from left to right. Walking, running and other physical activities can be uncoordinated and the child could have difficulty with symmetrical movements of the hands and feet. A strongly retained ATNR may eventually cause physical problems in the child's bone development. It may affect joints as well as the skeletal structure. It is often seen in children with scoliosis (curving of the spine).

When assessing and identifying a child with a retained ATNR, therapists will look for key features that indicate the child has retained the reflex. It may be mild and difficult to detect, or strong and obvious. If the child displays three or more of the following symptoms, further investigations should be conducted:
- Difficulty with visual tracking and crossing the mid-line.
- Difficulty with reading and following a line of text. Easily losing their place when reading. Difficulty reading small print.
- Listening skills and attention skills are difficult to develop.
- Difficulty with binocular vision so that images are blurred. Double vision as two eyes can't work together well.
- Poor handwriting and difficulty copying written script. Tight pencil grip.
- Difficulty with spellings.
- Poor eye-hand coordination.
- Difficulty with bilateral coordination.
- Poor sense of direction.
- Difficulty catching and throwing balls. Often using one hand to throw.
- Poor gross motor coordination and balance.
- Difficulty with swimming, especially breast stroke.
- The child finds it hard to tell their left from right.
- Poor short term memory and difficulty following verbal instructions.
- Impulsive and emotionally immature for their age.
The retained ATNR is often thought to be associated with dyslexia and attention deficit disorder. If a child is having marked difficulties with the above areas they would need an assessment to determine if the ATNR reflex has been retained. Occupational therapists use a variety of methods to test for the reflex. This ranges from a quantitative rating scale that indicates the degree of integration of the ATNR in normal first and third grade children for comparison; to Sensory Integration clinical observation assessments as well as observations of the child performing daily functional activities.
The ATNR can be integrated with therapy in which a series of exercises, specific games and activities are used. The activities involve movements which replicate the early reflex movements and therefore lay down the neural pathways that will enable the child to overcome the retained reflex. With young babies over 7 months a simple exercise would be to work with them on their stomach (prone position) reaching for toys in front and to either side of them. With young children, games can be used that involve e.g. crawling with their head turned to one side (tuck a bean bag or small soft ball under the chin between the shoulder). This can be done as a race. Simple exercises can be done with older children such as one handed wall push ups (standing sideways to the wall) with one hand on the wall and the other hand on the hip as the child faces away from the wall.
Once the child has integrated the ATNR improvements in classroom performance will be noticed providing there are no further underlying conditions or difficulties. Progress is different for each child and the activities should be done under the supervision of your therapist to ensure success and desired results.
USEFUL LINKS:
http://www.pediatricdevelopmentcenter.com/newsletters/Newsletter%20May08.pdf
http://www.primarymovement.org/background/index.html
write a comment …











/image%2F1484276%2F20151001%2Fob_ae1435_dsc02009.JPG)