Occupational therapy for children is 7 years old today! I hope to write more posts in the very near future. Keep watching this space!

Occupational therapy for children is 7 years old today! I hope to write more posts in the very near future. Keep watching this space!

Superstar Arts are committed to delivering high quality, meaningful, creative projects for young people and adults with learning disabilities. Their fundraising film is an appeal for help to keep the project running and to continue providing the quality of service for vulnerable young adults that they do today.
Dr. Frederick Covington (Occupational Therapist) Has composed and put together this video to show the diversity of the profession around the world. Occupational Therapists can be found in many different settings working towards our underlying goal of enabling individual people.
The I AM OT project has brought together many dedicated Occupational Therapists from around the globe, highlighting the countless specialist fields of prictice and showing a number of the highly skilled individuals involved. Many thanks to Dr. Frederick Covington.
Lauren is a brave 15 year old girl with Cerebral Palsy. In October she gave a speech at The American Academy of Cerebral Palsy and Developmental Medicine. This was not an easy task for her, but she spoke clearly and bravely.
Lauren's grandfather John has kindly agreed to have this video posted. Please take some time to watch this moving video.
To read about Lauren's dream and her journey to raise awareness and funds for Cerebral Palsy (CP) please take a look at the following link:

We all use our mouths in different ways throughout the day. We may use them to comfort ourselves (sucking a sweet, sucking your thumb, biting nails or just touching your mouth when stressed); to regulate and organise ourselves or to help maintain attention (chewing gum, chewing the end of a pen or pencil, taking deep breaths, blowing, whistling, biting your lip etc.). We also use our breath to help regulate and organise ourselves. The way we breathe in response to stimuli from our environment can help us to process the stimuli better. It can also assist in the activities we do daily.
Touch receptors (cells that give your brain information about the world around you through touch) are located all around your body. The lips and the fingers are considered to have the most concentration of touch receptor cells in the body. They correlate to a larger area of the brain that receives messages from the lips and fingers compared to other less sensitive areas of the body that correlate to smaller areas of the brain. More brain power is spent interpreting touch sensations from the lips and fingers than from other areas of the body that have touch receptor cells. Touch receptors help us to experience hot, cold, pain or pressure. Touch is an important sense because without it we would not recognise pain (e.g. from boiling water) and this would put us at great risk. Touch processing is very closely linked to emotional development which can also affect healing and the reduction of anxiety and tension. It has a great impact on a child's physical and psychological well-being.








Spatial awareness is the ability to be aware of oneself in space. It is an organised knowledge of objects in relation to oneself in that given space. Spatial awareness also involves understanding the relationship of these objects when there is a change of position. It can therefore be said that the awareness of spatial relationships is the ability to see and understand two or more objects in relation to each other and to oneself. This is a complex cognitive skill that children need to develop at an early age. Spatial awareness does come naturally to most children but some children have difficulties with this skill and there are things that can be done to help improve spatial awareness.
When a child is developing their spatial awareness they begin to become aware of their placement in relation to the things around them. They are central to this, and they need to understand their location as well as concepts like distance, speed and placement (over, under, behind etc.). Spatial awareness is part of our overall perception. The development of perception can be difficult for children with developmental co-ordination disorder (DCD), autism, cerebral palsy and many other conditions. As perception is the organisation and interpretation of sensory stimuli from our environment, the child would need to have adequate body awareness to be able to form the relationship of their body with the the stimuli and objects within that space. This is key to developing spatial awareness. Proprioception is the awareness of where our limbs are in space. This is developed alongside spatial awareness. For example, when a baby reaches for a toy it learns how far it needs to stretch the muscles in it's arms (proprioception) in order to reach the distance of the toy (spatial awareness). The next time the baby reaches for that toy it would have learnt something about the amount of muscle stretch needed and the distance of the toy. This can then be applied to a similar object at a similar distance another time. The child will eventually become familiar with where its limbs are without having to look at them. Distances, speed and placement will be integrated so that the child will know what they can reach and can't reach when they stretch their arm.

As spatial awareness develops the child will learn the concepts of direction, distance and location. They will understand that when they walk to an object the object will become closer to their body. they will know that objects that are far away appear smaller because of the distance. They begin to appreciate the space around themselves and the proximity of others around them. As they grow older their movements become more controlled and constrained around others as they are more aware of their personal space.
Children with poor spatial awareness tend to have visual perceptual difficulties as well. They may appear clumsy and may bump into others. They often stand too close or too far away from the people or objects that they are interacting with. In the classroom they may have difficulty with presentation of written work and may find it hard to structure and organise such work. These children often find it hard to tell their left from right and they confuse positional language i.e. over, under, in or out, left or right. This makes it hard for them to follow directions that use such language. They may have difficulty with PE, team games and games that use apparatus.
In the classroom the child with spatial awareness difficulties often finds mathematics hard. This is due to the abstract concepts of the subject especially where shapes, areas, volume and space is involved. They will have problems reproducing patterns, sequences and shapes. Their strengths, however, are with the more practical and concrete subjects. These children will often find that they excel at using a multisensory way of learning. They tend to have good auditory memory skills and have strength in speaking confidently whilst being able to listen well. They tend to have good verbal comprehension skills and their strength is usually in verbal and non verbal reasoning.

In order to be able to relate ourselves to objects in a given space, we need to have an accurate body schema. This is a sense of where your body is in space and where it is in relation to the whole of you. For example we need to know the exact location of our arms in relation to our trunk. The body schema develops through our muscles and touch receptors (proprioception and tactile senses combined with other senses). This gives us a map or image of the way we perceive ourselves to look and is linked with our body awareness. Asking a child to draw a picture of a person will give a trained therapist a very good indication of the child's body schema and it will provide the therapist with information on the child's spatial awareness. The therapist can also detect spatial awareness difficulties in a child's handwriting. A child with poor spatial awareness may leave out the spaces between words, start the sentence in the middle of the page, have difficulty keeping on the line or write diagonally instead of horizontally. These are visual perception problems that are related to spatial awareness.
An occupational therapist will also be able to identify a child with spatial awareness difficulties when observing their gross motor skills. The difficulties may be seen during team sports such as football where the child needs to judge distance and speed of a ball coming towards them, as well as the distance between themselves and the person they need to kick the ball to. They may also appear clumsy, move into spaces that they are not meant to be in during the game and often bump into team members.
Spatial awareness develops naturally when children have the ability to freely explore their environment. Babies learn about themselves and how they relate to their surroundings naturally. They learn to manipulate objects as they become mobile and learn about distances and sizes when they are able to move towards the objects. There are, however, situations that interfere with or prevent the natural development of spatial awareness. The child may have some developmental difficulty or a disability that results in poor spatial awareness. In other circumstances there may have been a lack of opportunity for the child to freely explore the environment during it's early developmental stages. The child may have been ill at key developmental points or may have missed opportunities for other reasons.

Occupational therapists work closely with parents and schools to provide suitable remedial exercises for a particular child with spatial awareness difficulties. The activities may involve games that work on judging distance and placement such as throwing beanbags into hoops, buckets or over lines (target games). They may use obstacle courses to involve the body and help the child to be aware of where they place their limbs in relation to the obstacles. Music and movement helps with placement, co-ordination and use of space. Games such as bowls or marbles help the child to develop a judgement of space.
At home parents can help to develop spatial awareness in the following manner:

If a parent is concerned about their child's spatial awareness they should seek advice from their child's GP, school or health care professional.
http://childdevelopmentinfo.com/learning/spatial.shtml

The Asymmetrical tonic neck reflex (ATNR) is a primitive reflex that is found in new born babies and normally remains until around 6 months. It emerges in utero at around 18 weeks after conception and is usually identified and seen within the first 3 months after birth. The reflex is initiated when the head is turned to the left or the right whilst the baby lies on its back. The turning of the head causes the arm and the leg on one side to extend, whilst the limbs on the opposite side flex. If the head turns to the right, the right arm and leg will automatically extend whilst the left arm and leg both flex. It is often called the "fencing" reflex due to this pattern.
The purpose of the ATNR is to provide stimulation for developing muscle tone and the vestibular system whilst in the womb before birth. It also assist with the birthing process by inhibiting limb movement and slowing it down so that the baby uses a "corkscrew" movement through the birth passage. ATNR helps with eye-hand co-ordination and serves as a precursor to this skill. A retained ATNR can have a significant impact on a child's development and it is often thought to have a major effect on the child's physical, cognitive, social and emotional progress, thus affecting their ability to function well in school. The retained reflex will continue to influence limb movement every time the head is turned and will have physical influences that impact on all other areas.
The ATNR will interfere with a baby's ability to centralise and reach things within the mid line position of their body. Once this reflex is integrated (around 6 months) the baby begins to reach and have functional ability within the mid line of their body. A strongly retained ATNR will affect this ability so that the baby finds it difficult for hands, feet and eyes to cross the mid line. Visual tracking and eye pursuit of an object becomes difficult and this later results in difficulty with reading as the child can not easily make the rapid forwards and backwards eye movements (saccades) that are essential for reading. Writing will also be difficult due to this as well as due to the reflex causing the hand to involuntarily extend as the head is turned towards the hand. The child will find it difficult to maintain a pen grip and may compensate with a lot of pressure in a tight grip, causing cramps and making their writing messy and illegible. The child may also find it difficult to copy written work as their eyes will follow their hand and not the text.

The retained ATNR prevents a baby from developing certain physical cross pattern movements such as rolling over, crawling and later marching using alternative leg and arm. As they grow older the child may have atypical movement patterns and may draw circles backwards, clap downwards, use one hand more than the other whilst clapping, or may be very single handed in most activities. A strongly retained reflex in the legs can also affect balance as the child looks from left to right. Walking, running and other physical activities can be uncoordinated and the child could have difficulty with symmetrical movements of the hands and feet. A strongly retained ATNR may eventually cause physical problems in the child's bone development. It may affect joints as well as the skeletal structure. It is often seen in children with scoliosis (curving of the spine).

When assessing and identifying a child with a retained ATNR, therapists will look for key features that indicate the child has retained the reflex. It may be mild and difficult to detect, or strong and obvious. If the child displays three or more of the following symptoms, further investigations should be conducted:
The retained ATNR is often thought to be associated with dyslexia and attention deficit disorder. If a child is having marked difficulties with the above areas they would need an assessment to determine if the ATNR reflex has been retained. Occupational therapists use a variety of methods to test for the reflex. This ranges from a quantitative rating scale that indicates the degree of integration of the ATNR in normal first and third grade children for comparison; to Sensory Integration clinical observation assessments as well as observations of the child performing daily functional activities.
The ATNR can be integrated with therapy in which a series of exercises, specific games and activities are used. The activities involve movements which replicate the early reflex movements and therefore lay down the neural pathways that will enable the child to overcome the retained reflex. With young babies over 7 months a simple exercise would be to work with them on their stomach (prone position) reaching for toys in front and to either side of them. With young children, games can be used that involve e.g. crawling with their head turned to one side (tuck a bean bag or small soft ball under the chin between the shoulder). This can be done as a race. Simple exercises can be done with older children such as one handed wall push ups (standing sideways to the wall) with one hand on the wall and the other hand on the hip as the child faces away from the wall.
Once the child has integrated the ATNR improvements in classroom performance will be noticed providing there are no further underlying conditions or difficulties. Progress is different for each child and the activities should be done under the supervision of your therapist to ensure success and desired results.
USEFUL LINKS:
http://www.pediatricdevelopmentcenter.com/newsletters/Newsletter%20May08.pdf
http://www.primarymovement.org/background/index.html
 It is difficult for anyone who is not on the spectrum to understand the daily barriers that affect a person with autism. These barriers are due to their perception and experience of the world which can be so extreme as to prevent them from leading a normal life.
It is difficult for anyone who is not on the spectrum to understand the daily barriers that affect a person with autism. These barriers are due to their perception and experience of the world which can be so extreme as to prevent them from leading a normal life.
The National Autistic Society describes autism as:
"Autism is a lifelong developmental disability that affects how a person communicates with, and relates to, other people. It also affects how they make sense of the world around them. It is a spectrum condition, which means that, while all people with autism share certain difficulties, their condition will affect them in different ways."
Autism will not only have an impact on the way the person communicates and relates to others, it will also have a profound affect on the way the person responds to and interacts with the environment. This often manifests in their behaviour. It is a complex neurodevelopmental disorder that has multiple symptoms that begin before the child is 3 years old. These include:
These symptoms are variable in their severity from one individual to another. This results in the use of the term "spectrum".
Children with autism have difficulty making sense of the world. This is mainly due to them having difficulty processing the sensory stimuli from their environment which can cause them a great amount of anxiety. the world is a confusing place for them and they are often over loaded with sounds, smells, sights, tastes and sensations that may appear vivid and extreme, disjointed, or even lacking in some way. These children will try to create some sort of order for themselves so that they can gain a feeling of security in the total chaos they experience daily.

The difficulty they have in processing daily sensory information is referred to as Sensory Processing Disorder. It can cause a great amount of stress and anxiety as well as inappropriate or difficult behaviour. They may feel physical pain at times and find that they are unable to express this in words. They often either shut down, or react to the over load of stimuli. Sensory Processing Disorder can result in the person being hypersensitive or hyposensitive to stimuli whereby they can over react or under react to e.g. sound, touch or light.
The main areas of processing difficulties are seen when a child is hypersensitive or hyposensitive to the seven senses which are sight, sound, touch, taste, smell as well as balance (vestibular) and body awareness (proprioception) - see previous posting on Sensory Integration (1 and 2). The results of these sensitivities are seen in the person's behaviour. For example, a child with hypersensitive vision may see fragmented images, or their vision may be distorted where objects and bright lights appear to jump about. They may find it easier to focus on one spot of detail rather than take in the whole scene as this could be too overwhelming especially if it is distorted, too bright and fragmented. the child may not want to look directly and people and may often find it difficult to have eye contact. They may avoid certain rooms due to the lighting, wall colour, or objects in the room as it may heighten their sensitivity to a very uncomfortable level. The resulting behaviour often appears unrelated to anything obvious within the environment and this can result in parents and carers remaining confused and unsure how to help their child. This is an example of one of the senses, but there is often a combination of processing difficulties involving two or more senses.
There is no cure for autism, however, there are several treatment and management approaches that can help to make a difference to the child's life. These range from simply adjusting the child's diet to a combination of therapies, behaviour interventions and self help tools. The approach taken will depend on the individual and their level of needs. Before deciding on any approach it is essential to gain sufficient knowledge of its aims. The approach needs to be positive and motivating, whilst building on the child's strengths. It should enable the child to reach their full potential for a better quality of life.
http://www.youtube.com/watch?v=Haw5m3Zxvy4&feature=player_embedded
http://media-dis-n-dat.blogspot.com/2010/10/service-dogs-may-reduce-stress-in.html
http://www.sensory-processing-disorder.com/10-things-every-child-with-autism-wishes-you-knew.html
http://www.youtube.com/watch?v=a3Xp__PdexU&feature=youtu.be
http://www.handsinautism.org/pdf/How_To_SensoryKits.pdf
 What is it?
What is it? A child with dyspraxia can present with a wide spectrum of difficulties. The term is, however, used to describe co-ordination difficulties with evidence of significant perceptual problems in the majority of cases. Caution should be taken when using the term as it may eventually be loosely applied to every child who shows a little forgetfulness, disorganisation and clumsiness in their daily routines. Children develop at different rates and this should always be taken into consideration when looking at individual cases.
The term dyspraxia is taken from the Greek word duspraxia. Duspraxia is formed of dus (or dys) and praxia(or praxis which is taken from an older Greek word prassein).Praxis is to practice an act or a function, pass through, experience; therefore "to act". Dys means impaired, ill or abnormal, so the literal meaning of dyspraxia is ill-doing or abnormal act.
Developmental dyspraxia is an immaturity of the organisation of movement. The brain does not process information in the way that allows the full transmission of neural messages. A child with dyspraxia will find it hard to plan what to do and how to do it. Dyspraxia is also known as Developmental Co-ordination Disorder (DCD), Perceptual-Motor Dysfunction, and Motor Learning Difficulties. The terms Clumsy Child Syndrome or Minimal Brain Damage are no longer used.
Children and adults with dyspraxia find it difficult to learn how to plan and co-ordinate their movements. the condition is therefore also known as a "motor learning disability". Someone with dyspraxia will find it hard to carry out smooth and co-ordinated movements because the simultaneous perceptual and motor processes of carrying out an act successfully is a complex task that requires conscious imaging, planning, positioning, balance, muscle activation and co-ordination.
Dyspraxia often comes with language problems and sometimes a degree of difficulty with perception and thought. Dyspraxia does not affect a person's intelligence, but it can cause difficulties with learning, especially for children.
For the majority of people with dyspraxia there is no known cause. Current research suggests that it is due to an immaturity of neuron development in the brain. It is not a result of brain damage and people with dyspraxia have no clinical neurological abnormality that would explain the condition.
When considering the brain, the cerebral cortex (the upper most part of the brain) receives impulses from sensory organs through a network of nerve fibres passing from the brain stem. As a child grows and learns, the connections between the nerve cells (neural pathways) become established and reinforced with successful learning. When a child learns a series of movement patterns the repetition of movement reinforces the pattern so that its planning is almost reflex. The use of external sensory input such as sight and sound together with the learned movement patterns will enable the cerebral cortex to judge the best course of action and send out appropriate motor impulses.
The cerebral cortex is divided into a right hemisphere and a left hemisphere. Each side has different functions and operates quite separately. Some functions are shared, but the sides generally work independently to provide its information that is brought together to complete the whole picture e.g. the left hemisphere receives the information in a jumbled, disjointed way and
needs to work well together with the right hemisphere so that the information, images and actions are interpreted correctly for the right results.
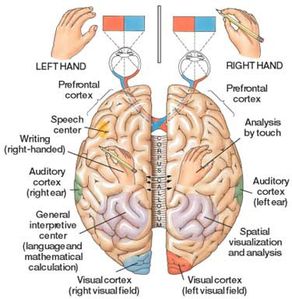
In children with dyspraxia, the two hemispheres of the cerebral cortex are not working in harmony to produce the desired results. The basic development of the hemispheres appear reduced, and as they determine whether a person is right or left handed, you will often find that children with dyspraxia will use both hands without developing a dominant hand for some time. This affects fine motor activities even further e.g. handwriting skills.
The cerebral cortex also surrounds the "thalamus", "hypothalamus" and "pituitary gland of the limbic system. The limbic system is responsible for the instinctive and automatic responses with the body and it is closely linked to emotional behaviour. A mature cerebreal cortex would be able to dampen down the limbic system's emotional response to external stimuli. If the cerebral cortex does not mature as expected, the individual would be excitable, over emotional and extremely sensitive to external sensory input.
The symptoms of Dyspraxia can be evident from an early age. Babies may be irritable from birth and may exhibit significant feeding problems. They are slow to achieve expected developmental milestones. For example, by the age of 8 months they may still not be able to sit up independently. Many children with dyspraxia fail to go through the crawling stage, preferring to "bottom shuffle" and then walk. Later, they will avoid tasks that require good manual dexterity.
The essential features of dyspraxia are often linked and associated with Developmental Co-ordination Disorder (DCD). The two are often considered the same. This can be confusing and the terminology used may depend on which country you are living in. There are, however, some inherent differences between dyspraxia and DCD. Dyspraxia has been generally considered under the umbrella term of DCD which is outlined below as defined in the DSM-IV. A diagnosis of DCD can be made if the following criteria are met:
A marked impairment in the development of motor co-ordination
The impaired motor co-ordination significantly interferes with academic achievements or activities of daily living
The significant motor co-ordinationdifficulties are not due to general medical conditions such as cerebral palsy, hemiplegia or muscular dystrophy and the criteria are not met for Pervasive Developmental Disorder.
If mental retardation is present, the motor difficulties are in excess of those usually associated with it.
The difference between DCD and dyspraxia is that: "The term DCD describes a more generalised motor co-ordination difficulty which shows a marked difference between the levels of skills that would be expected for age or level of intelegence and significantly interferes with academic or activities of daily living. This is not caused by another medicalcondition (for example cerebral palsy) and it is not part of a pattern of general learning difficulties. The term dyspraxia describes an immaturity of the development of the organisation and sequencing of movement. It can also affect speech, perception and thought. Not all people with DCD have dyspraxia, but often the words are used interchangeably. Difficulties associated with both DCD and dyspraxia have an impact on living and learning in all areas of a child's life, at home, school and at play."Dyspraxia Foundation.

Jean Ayres (1965) defined dyspraxia as a disorder of sensory integration interfering with the ability to plan and execute skilled non-habitual tasks. The child with dyspraxia has a praxis/planning problem and does not know how to move, whereas the child with DCD has difficulty with co-ordination and execution. the child with DCD knows what to do, but does not do it very well. There is still some debate over terminology and the term dyspraxia tends to be used more generally in the UK.
The infant school child with dispraxia could display the following symptoms:
The junior and senior school child will probably continue to have the difficulties experienced by the infant school child with little improvement if their needs are not addressed by this stage. It is unlikely that major changes in their ability would occur, but they can make good progress in school with understanding, support and good coping strategies. children with dyspraxia may lose self confidence and motivation as they find school work increasingly difficult. By the time they reach secondary school their attendance record is often poor.

Occupational therapists are able to assess children with movement and co-ordination problems to determine the exact nature of the difficulties and how it impacts the child's day to day life. The intervention will focus on how the child manages daily activities at home, school and play and it will work on the assumption that children develop skills as a consequence of the interaction between the child, the environment and the task.
The use of Sensory Integration techniques will focus on the underlying impairment of which the treatment will aim to improve the functional performance.
The main areas of the school curriculum that children with dyspraxia struggle with are in the areas of literature, handwriting, mathematics and PE. Children with dyspraxia have difficulty with concentration and listening skills. They may have literal use of language and this will affect their reading and spelling ability. They may read well, but not understand some of the concepts in language. Some exercises such as those in Take Time by Mary Nash-Wortham and Jean Hunt may provide help in these areas. Computers can provide support and the Wordshark 2 is a programme available from the Dyspraxic Foundation.
Poor handwriting is one of the most common symptoms of dyspraxia. A child with poor handwriting does not need to be told that their writing is bad. They can see that they are not as good as their friends. It is important therefore to concentrate on the positive rather than the negative. Please see my previous posting on Handwriting for ways to support handwriting difficulties.
The following is a list of assessment tools often used by occupational therapists:
Perceived Efficacy and Goal Setting System (PEGS) Developed by MissiunaC, Pollock N, and Law M (2004) Available from The Psychological Corporation/Harcourt Assessment
Assessment of Motor and Process Skills (AMPS) and School Assessment of Motor and Process Skills (School AMPS) For information see www.AMPS-UK.com
Pediatric Evaluation of Disability Inventory (PEDI) – for children up to 7.5 years of age. Developed by Hayley et al(1992) available from The Psychological Corporation/Harcourt Assessments
Movement Assessment Battery for Children (Movement ABC). Developed by Henderson S and SugdenD (1992) available from The Psychological Corporation/Harcourt Assessment
DevelopmentalTest of Visual Motor Integration (VMI) developed by Beery K, Buktenica N, Beery N (5th Edition 2004) Available from Ann Arbour Publishers and nferNELSON
Bruininks-Osteretsky Test of Motor Proficiency developed by Bruininks R, (1978) published by American Guidance Service
Test of Visual Perceptual Skills – non-motor (TVPS) developed by Gardner M (1996) available from Ann Arbour Publishers
Motor-Free VisualPerceptual Test (MVPS) developed by Mercier L, Hebert R, Collarusso R, Hammil D (2002) available from Ann Arbour Publishers
Sensory Profile developed by Dunn W (1999) available from Harcourt Assessment (see also www.sensoryprofile.com)
Ammendment:
On a recent course hosted by the COT (college of Occupational Therapists) it was considered that DCD is the official medical diagnosis of which dyspraxia is a symptom ("Is it DCD or isn't it?" Dido Green and Carolyn Dunford 16th April 2012 - London) - amendment added 24/04/2012.
http://www.dyspraxiafoundation.org.uk/info/about_us.php
www.fhs.mcmaster.ca/canchild/
Includes handouts on cognitive approaches to intervention, fine motor difficulties,
http://mastersinoccupationaltherapy.org/2011/11/
For 40 best online tools for occupational therapists
 Babies learn to move around and investigate their environment as part of their natural developmental process. They begin by rolling, shuffling, sitting and finding different positions to reach objects or to move towards an object. Natural curiosity and a need to explore will result in more effective ways of getting around. At about 6 to 8 months a baby will learn to balance on their hands and knees and will gradually learn how to move forwards and backwards by pushing off with their hands and knees. Crawling usually happens at around 9 or 10 months, but some babies never crawl and find other methods to move around such as bottom shuffling or sliding on their tummies.
Babies learn to move around and investigate their environment as part of their natural developmental process. They begin by rolling, shuffling, sitting and finding different positions to reach objects or to move towards an object. Natural curiosity and a need to explore will result in more effective ways of getting around. At about 6 to 8 months a baby will learn to balance on their hands and knees and will gradually learn how to move forwards and backwards by pushing off with their hands and knees. Crawling usually happens at around 9 or 10 months, but some babies never crawl and find other methods to move around such as bottom shuffling or sliding on their tummies.
The Importance of Crawling
As a baby crawls he is learning to move around the environment on his own and therefore has a sense of independence. The baby can decide where he goes and he will start to develop decision making skills based on movement which include motor planning. His muscles are being strengthened in preparation for walking and he is using the limbs on either side of the body to develop bilateral co-ordination.
Crawling is seen as an important developmental milestone in terms of brain development. Some links have been made with the lack of crawling and dyslexia, poor co-ordination, ADHD and other similar problems in healthy children. There is, however, no proven evidence to support the link between not crawling and these conditions. Children with physical issues that prevent crawling have pre existing problems which cause them not to crawl. It is not the lack of crawling that causes these problems. Retained infantile reflexes such as the symmetric tonic neck reflex can cause many problems including learning difficulties. The underlying problem causes the lack of crawling and not the other way round.

Benefits of Crawling
Crawling has many benefits as it is part of the natural developmental progress to standing, walking and running. A baby needs to learn to lift its body off the floor whilst on all fours and maintain that position. This helps to align the spine and develop the muscles of the back, hips and shoulder girdle in preparation for standing.
Crawling is beneficial for many reasons which include social, emotional, motor, cognitive, sensory and personal (well being) factors. While crawling a baby will be able to connect with his parents in new ways. He can check to see where they are by turning around and looking back whilst crawling away. This develops a stronger 'self' identity and increases his independence. The baby will also be able to discover that things exist far away from him. He gains experience necessary to calibrate how far away an object really is, developing visual skills as well as perception e.g. the more crawling it takes to reach an object, the further away it is, and vice versa. He also learns how to navigate his environment and will learn from the environment as he notices and experiences new things.
Crawling helps to develop balance, strengthen muscle tone and develop eye-hand co-ordination. This is necessary for future reading writing and physical activities. Bilateral integration is improved through crawling as both hands, legs, eyes and ears are required to work in synchronisation, increasing left and right brain co-ordination. The crawling movement is repetitive and this stimulates brain activity to develop cognitive processes such as concentration, memory, comprehension and attention.

Sensory Processing
Crawling allows for the integration of sensory information. This allows the baby to have a complete picture of his environment. He learns spatial concepts and develops the visual and auditory systems. As the baby crawls he will use both ears simultaneously for reception to develop binaural hearing. Both eyes are also used to begin to develop binocular vision.
Crawling stimulates the inner ear of the vestibular system whilst the baby moves forwards (or backwards) and moves his head. This will help improve balance. Crawling will also give the baby sensory stimulation through his hands and knees as he weight bears through them. This is essential for gross and fine muscle development. He will also receive different tactile sensations as he crawls over different textured surfaces.
Not all movement 'styles' or variations on crawling give the same developmental benefits as the 'traditional' crawling movement pattern. Normal crawling uses both arms and legs alternatively to move. The movement is forward, however, backward movement is often seen when babies are just learning to crawl and that is normal.
Helping Babies to Crawl
Babies develop skills differently and some learn quicker than others. If a baby does not show interest in crawling or moving around (creeping, scooting, shuffling etc.), then they should be encouraged and enticed by placing objects out of their reach or by calling them to you. Most babies who have had plenty of Tummy Time will find crawling to be a natural progression because they are used to being on their tummy and have pushed up with their arms may times in preparation for movement. There may be underlying physical or neurological reasons why a baby will not be able to crawl, or it may simply be due to environmental or motivational factors.

There are many toys and stimulating object on the market to encourage our little ones to crawl. there are also ways to help and assist children with special needs to move about appropriately at that developmental stage. The baby may just need a small amount of encouragement by doing something different like getting down on the floor with him, laying him on his stomach and assuming the same position in front of him where he can see you. This may provide enough encouragement and incentive for your baby to want to move towards you. If your baby is not crawling by 12 months and has not moved on to standing or walking, then professional advice should be sought.

Useful Links:
http://www.centeredge.com/ArticPDF/STNR.pdf
/image%2F1484276%2F20151001%2Fob_ae1435_dsc02009.JPG)